Mental Health and the role of Psychedelics
Part 1 of a series of articles on the use of psychedelics to treat mental health conditions.
Psychedelics and the Mental Health Crisis
This will be the first in a series of articles to discuss the current mental health crisis and how psychedelics can help improve treatment outcomes and potentially be one of the most significant breakthroughs in mental health treatment in decades.
The mental health crisis has become a significant public health concern in recent years. Mental illnesses affect millions in North America, and the economic, social and human costs associated with these conditions are staggering. According to Statistics Canada, in any given year, 1 in 5 Canadians experiences a mental illness, and by the age of 40, almost 50% of Canadians will have or had a mental illness.
Despite significant efforts to address this crisis, the current standard of care has been unable to keep pace with the growing demand for mental health services. We will explore the causes and consequences of the mental health crisis and examine the current standard of care and its efficacy.
Causes of the Mental Health Crisis
Many factors contribute to the mental health crisis. One of the primary causes is the lack of access to mental health services. In Canada and the United States, many people who suffer from mental illnesses do not receive the care they need due to a shortage of mental health professionals, inadequate insurance coverage, or long wait times for treatment. This lack of access to care can lead to worsening symptoms, increased disability, and even suicide.
Recent studies suggest that excessive or problematic use of social media can negatively impact mental health, including increased feelings of loneliness, anxiety, depression, and stress. However, it's important to note that the relationship between social media use and mental health is complex, and more research is needed to understand the mechanisms at play.
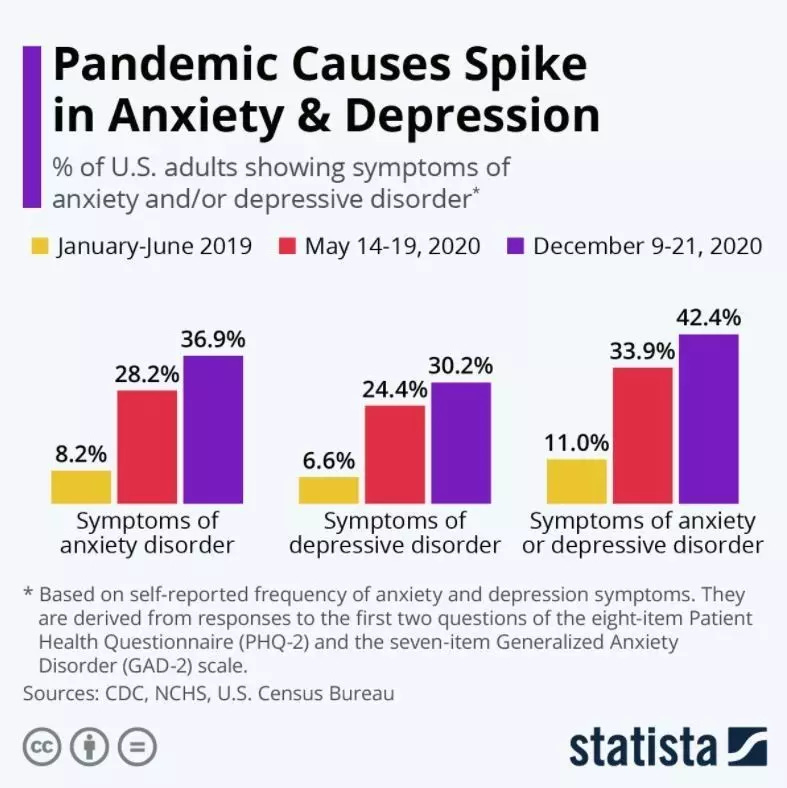
The COVID-19 pandemic also has had a significant impact on mental health globally. The pandemic has caused widespread fear, anxiety, and stress due to economic uncertainty and social isolation. Studies have shown that the pandemic has increased mental health problems such as depression, anxiety, and post-traumatic stress disorder (PTSD).
Economic Costs
The economic and social costs of the mental health crisis are significant. According to an Open Minds Market Intelligence report, spending on mental health treatment and services in the United States reached $225 billion in 2019 and had grown 52.1% over the preceding decade. In Canada, the annual economic costs for mental health care are estimated to be over $50 billion.
According to a report in The Lancet, “lost productivity due to two of the most common mental disorders, anxiety and depression, cost the global economy US$ 1 trillion annually. In total, poor mental health was estimated to cost the world economy approximately $2·5 trillion per year in poor health and reduced productivity in 2010, projected to rise to $6 trillion by 2030.”
Human Costs
Mental health problems can cause immense suffering and negatively impact an individual's quality of life. Mental illnesses such as depression, anxiety, and PTSD can affect a person's thoughts, emotions, and behaviours, making it difficult to function normally. The human cost of mental health problems is profound and includes lost opportunities, family breakdown and decreased life expectancy. In Canada, mental illness is the second leading cause of disability. In addition, substance abuse accounts for approximately 47,000 deaths in Canada annually.
SSRI/SNRIs
SSRIs (Selective Serotonin Reuptake Inhibitors) introduced in the late 1980s and SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) introduced in the 1990s are commonly prescribed medications for treating mental health issues, including anxiety, depression, and other related disorders. These medications increase neurotransmitters, such as serotonin and norepinephrine, in the brain, which can help to improve mood and decrease anxiety.
These medications are often the first-line treatment for depression, anxiety, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD). A large study published in The Lancet has shown that SSRIs are more effective than placebo in treating acute depression, but scientists continue to debate the efficacy of these drugs. These medications are generally well-tolerated and have fewer side effects than older antidepressants, such as tricyclic antidepressants.
However, it is essential to note that while SSRIs and SNRIs can be effective, they are not a one-size-fits-all solution. Not all patients respond to these medications; some may experience debilitating side effects, such as nausea, weight gain/loss, and sexual dysfunction, while others need to try several different drugs to find one that is acceptable.
It is also worth noting that these medications may take several weeks to start working, and patients may need to be on them for an extended period to see full benefits.
The global antidepressant drugs market was valued at $15,651.0 million in 2020 and is projected to reach $21,004.8 million by 2030, registering a CAGR of 3.0% from 2021 to 2030.
In summary, SSRIs and SNRIs can effectively treat anxiety, depression, and other mental health conditions in many patients. However, the efficacy and safety of these medications may vary depending on the individual and their specific situation. Better options for those suffering from mental health issues must be provided.
Enter Psychedelics
Psychedelic drugs, such as LSD (lysergic acid diethylamide), psilocybin (found in certain mushrooms), and MDMA (3,4-methylenedioxymethamphetamine), have a long and somewhat controversial history of use in the treatment of mental health disorders, including addiction. While these substances were initially studied in the 1950s and 1960s, research on psychedelics was halted in the 1970s due to the War on Drugs and government restrictions. However, recent advances in research have led to renewed interest in the therapeutic potential of these drugs.
In the 1950s and 1960s, psychedelics were studied for their potential to treat various mental health disorders, including depression, anxiety, and addiction. Early research suggested that these substances could help individuals achieve altered states of consciousness that could facilitate profound psychological experiences and insights. Some researchers believed that these experiences could help patients break free from negative patterns of thought and behaviour and lead to lasting positive changes.
One of the most well-known researchers was Dr. Timothy Leary, who researched psychedelics at Harvard University in the 1960s. Leary and his colleagues believed that psychedelics could transform society and promote greater empathy and understanding among individuals. However, their work was controversial and eventually led to increased government restrictions on the use of these substances.
In recent years, there has been a resurgence of interest in the therapeutic potential of psychedelics, particularly in treating addiction, depression and PTSD. Studies have suggested that substances such as psilocybin and MDMA may be effective in helping individuals overcome addiction to drugs such as opioids and alcohol.
A study published in JAMA Psychiatry in 2022 found that individuals who received psilocybin-assisted therapy for alcohol use disorder had a higher rate of drinking reduction than those who received an active placebo combined with psychotherapy. Similarly, a small study published in Nature in 2021 showed MDMA was effective in reducing symptoms of post-traumatic stress disorder (PTSD).
While the research on psychedelic drugs in treating mental health disorders is still in its early stages, there is growing interest and funding for this study area. In recent years, the U.S. Food and Drug Administration (FDA) has granted "breakthrough therapy" designation to MDMA-assisted psychotherapy for PTSD and psilocybin for treatment-resistant depression. This designation is intended to expedite the development and review of these treatments.
In conclusion, the research history of psychedelic drugs in treating mental health disorders, including addiction, is a complex and sometimes controversial topic. While early studies suggested that these substances could have profound therapeutic effects, research was halted mainly in the 1970s due to government restrictions. However, recent advances in research have led to renewed interest in the therapeutic potential of these substances, particularly in the treatment of addiction. While the investigation is still in its early stages, there is growing interest and funding for this area, and some studies have shown promising results, which we will discuss further in later posts.
Mental health costs are multiplying and are a leading cause of disability globally. Finding effective treatments with fewer side effects will be critical for trying to get this crisis under control. Psychedelics could fit the bill for several mental health and addiction issues, which we will dive into in future posts.
.